
Body Contouring Experience
1,000 Breast Revisions
The Beverly Hills Shape®
The Dr. Oz Show™

Beverly Hills Board-Certified
Plastic Surgeon To The Stars
-
Specializes in Implant Explantation including En Bloc Capsulectomy
-
Placed Over 14,000 Breast Implants
-
Over 25 Years of Body Contouring
-
Perform over 1,000 Breast Revisions
-
Medical Advisory Board, The Dr. Oz Show™
-
Patients from 46 countries
-
Creator, The Linder Bra®, Sold Worldwide
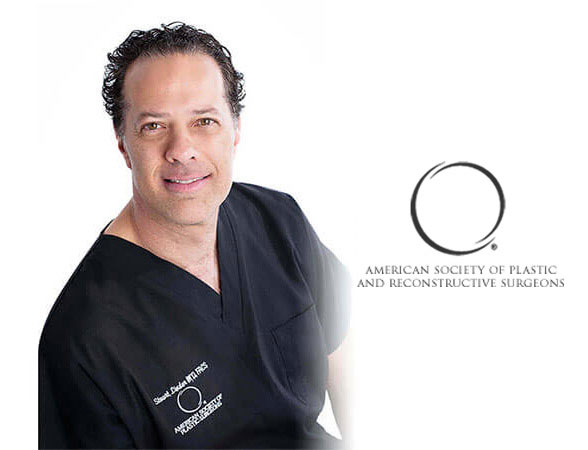
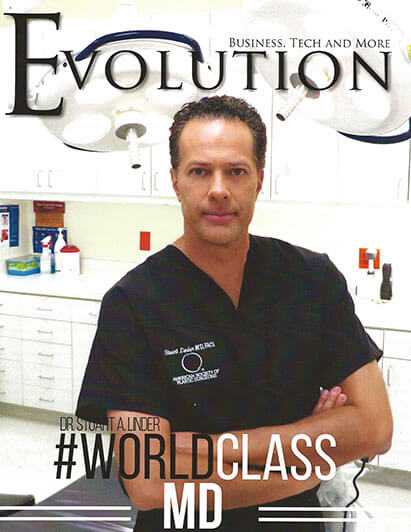
Dr. Stuart Linder is a Beverly Hills board certified plastic surgeon, specializing in body sculpting and reconstructive procedures including breast augmentation, breast reduction, breast lift, breast implant revision, liposuction and tummy tuck. He is board-certified by the American Board of Plastic Surgery and is affiliated with the American College of Surgeons, the American Society of Plastic and Reconstructive Surgeons and the American Medical Association.
Meet Dr. LinderDr. Linder specializes in all types of breast procedures and is one of the most sought after breast surgeons
View Over 4900
Before & After Photos
Browse through Dr. Linder’s comprehensive photo gallery for pre- and post-operative procedures.
Most Popular
View Photo Gallery
Breast Augmentation
"I had my breast augmentation with Dr. Linder a month ago and they look so beautiful. Thank you Dr. Linder for making me feel and look fabulous. I feel more comfortable under my skin. My girl friends are also very happy with there results. You are sure the best!"
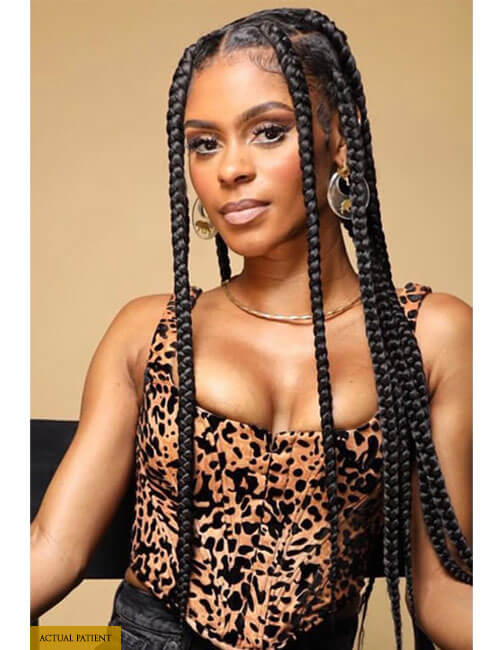
Tummy Tuck
"Dr. Stuart Linder is a very excellent surgeon in Beverly Hills. I had my tummy tuck done in the Phillipines and I am not happy with the job they did and Dr. Linder revised my tummy and it was ten times better and I’m happy and very satisfied of the result. I would highly recommend him he’s great."

Breast Revision
"It’s not the regular augmentations that are impressive, but his ability to correct/revise other surgeons mistakes. I don’t know where I’d be, mentally and emotionally, if it wasn’t for Dr. Linder fixing mine."

Liposuction
"You Made a difference. I sincerely would like to thank you for taking care of my liposuction needs. I am on top of the world with happiness and a renewed self-confidence."
Credibility
"Confident in Dr. Linder! I feel 100% confident w/ Dr. Linder. My health comes first & I trust it to be in good, expert, caring hands with him. The team and customer service is outstanding."
Dr. Linder appears on television regularly, including The Dr. Oz Show, The View, 20/20 with Barbara Walters, Discovery Health Channel, Extra, ABC, and Entertainment Tonight.

The Doctors
Plastic Surgery Body Contouring

The Insider
Beauty Secrets of Ageless Stars

ABC 20/20
The Cutting Edge With Barbara Walters

Kcal 9
Plastic Surgery Body Contouring

Entertainment Tonight
The Back To Work Makeover

The Style Network
Big Rich Texas

The Dr. Oz Show
Secrets to Cheat Your Age

The View
Plastic Surgery Interview and Appearances

The Doctors
Plastic Surgery Body Contouring

The Insider
Beauty Secrets of Ageless Stars

ABC 20/20
The Cutting Edge With Barbara Walters

Kcal 9
Plastic Surgery Body Contouring

Entertainment Tonight
The Back To Work Makeover

The Style Network
Big Rich Texas

The Dr. Oz Show
Secrets to Cheat Your Age

The View
Plastic Surgery Interview and Appearances
Voted Best Plastic Surgeon In Beverly Hills, CA
By the American Institute of Plastic Surgeons 2022
Full and shapely breasts are desirable to most women. Breast augmentation using implants is the best way to enhance a woman’s appearance and achieve a voluptuous, feminine look. Here, saline or silicone implants are placed to increase breast volume and improve breast shape. Dr. Linder has been performing this surgery for over two decades and has placed over 12,000 implants.
Learn MoreThere are several reasons a woman would need to return for a secondary breast surgery. Breast revision adjusts or corrects implant complications from a previous breast augmentation to restore a beautiful and comfortable breast aesthetic. Whether from an implant complication (like rupture or capsular contracture) or the desire to change implant sizes, breast revision can help. Dr. Linder performs breast revision on a weekly basis.
Learn MoreBreast sagging is a natural part of the aging process and is often made worse by pregnancy and weight loss. Breast lift surgery is performed to address this unwanted drooping of the breast. By removing excess skin and tightening underlying tissues, breast lift surgery can help restore a more youthful, perky appearance to the chest. This is commonly performed alongside breast augmentation.
Learn MoreDr. Stuart Linder Specializes in Breast Implant Removal (Explantation)
Total Capsulectomy
Learn More
Follow Dr. Linder
On Instagram
drstuartlinder
Board-Certified Plastic Surgeon in Beverly Hills, that specializes in breast augmentation, breast reduction, and breast revision procedures